A stroke is a life-altering event that can range from mild and recoverable to devastating and fatal. For some individuals, especially those who experience severe strokes, the damage to the brain and body may be so extensive that recovery is no longer possible. In these situations, families and caregivers are often faced with the painful reality of end-of-life care. Recognizing the signs of impending death after a stroke can help loved ones prepare emotionally, make informed medical decisions, and focus on comfort and compassion during a deeply challenging time. This article explains what a stroke is, how decline may progress, and the physical, neurological, and emotional signs that may appear as life draws to a close.
What is a Stroke?
A stroke occurs when blood flow to part of the brain is interrupted, depriving brain cells of oxygen and nutrients. This interruption may be caused by a blockage, known as an ischemic stroke, or by bleeding in the brain, known as a hemorrhagic stroke. The severity of a stroke depends on how large an area of the brain is affected and how quickly treatment begins. Mild strokes may result in temporary weakness or speech difficulties, while severe strokes can lead to permanent disability, loss of consciousness, or death. Risk factors such as high blood pressure, heart disease, diabetes, smoking, and advanced age increase the likelihood of experiencing a stroke, which is why prevention strategies like managing chronic conditions and recognizing early warning signs are so important.
Signs of Impending Death After a Stroke
When a stroke is catastrophic, the body may begin a gradual shutdown process. Understanding this progression can help families recognize that changes they are seeing are part of the natural course of decline rather than something they caused or failed to prevent. In many cases, the brain damage affects vital functions such as breathing, swallowing, and heart regulation. As these systems become less stable, the body conserves energy by reducing activity, leading to noticeable changes in physical and mental function.
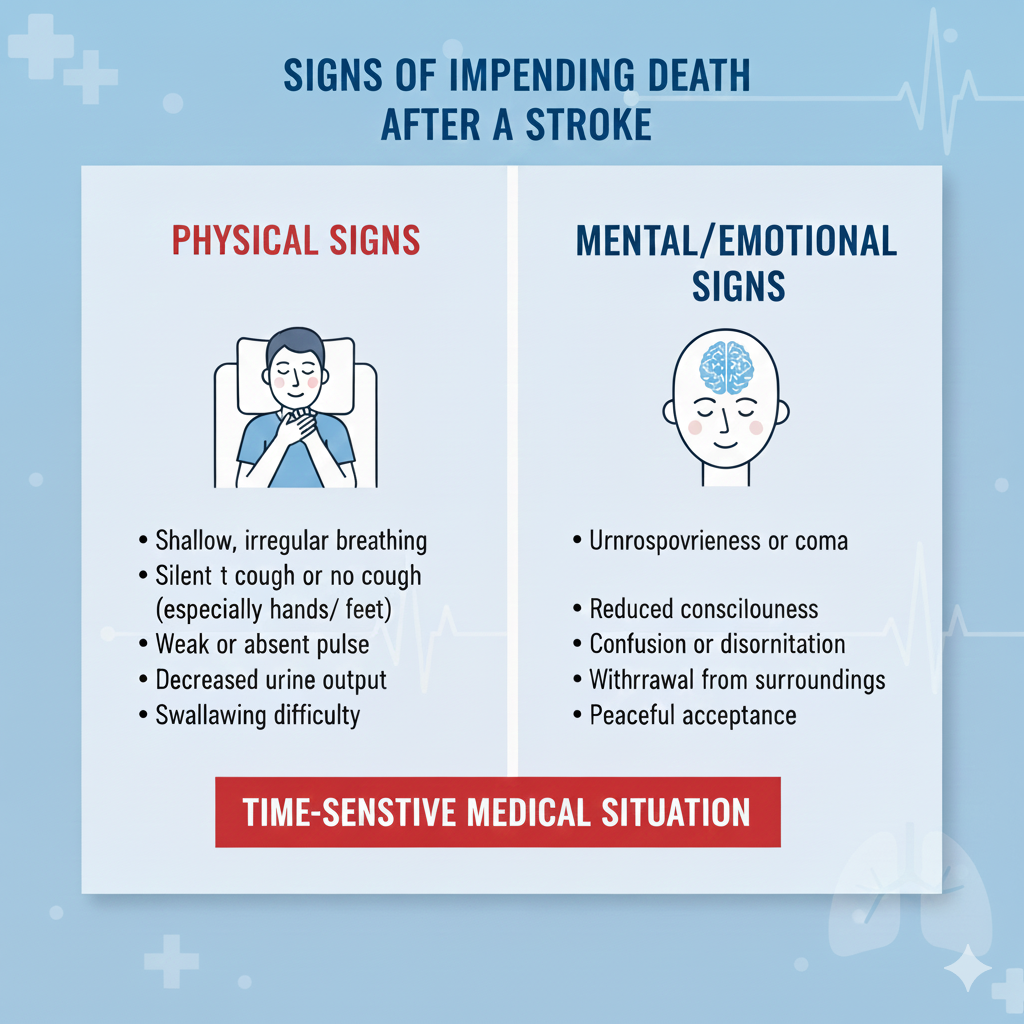
Physical Signs to Recognize
Physical signs are often among the first indicators that the end of life may be approaching after a severe stroke. Profound weakness or complete immobility is common, as the brain can no longer effectively control muscles. Difficulty swallowing, known as dysphagia, may worsen, increasing the risk of aspiration and making eating or drinking unsafe. Weight loss and dehydration may occur as the body’s demand for nourishment decreases. Skin may become cool or mottled, particularly in the hands and feet, as circulation slows.
Neurological Decline
Neurological decline is another major component of the dying process after a stroke. Many individuals become increasingly drowsy and may spend most of the day sleeping. Periods of confusion, disorientation, or unresponsiveness are common as brain function deteriorates. Speech may become slurred, minimal, or stop entirely. Some individuals may no longer recognize loved ones or respond to voices, although hearing is often believed to be one of the last senses to fade.
Respiratory Changes
Changes in breathing patterns are particularly significant signs of impending death. Breathing may become irregular, shallow, or labored, with long pauses between breaths. A pattern known as Cheyne-Stokes respiration, characterized by cycles of rapid breathing followed by periods of apnea, may develop. Congestion in the throat can cause a rattling sound, which can be distressing for family members but is typically not uncomfortable for the person experiencing it. Healthcare providers can offer guidance on positioning and medications to ease these symptoms.
Cardiovascular Symptoms
Cardiovascular symptoms also reflect the body’s gradual shutdown. Blood pressure may drop, and the pulse can become weak, irregular, or difficult to detect. The heart may struggle to maintain a steady rhythm as the brain’s control over vital functions declines. These changes often coincide with reduced urine output and swelling in the extremities, signaling decreased organ function.
Changes in Body Function
As bodily systems slow, there are also notable changes in overall body function. Temperature regulation may become impaired, causing the person to feel unusually warm or cold. Bowel and bladder control may be lost, and reflexes may diminish. These changes are not signs of suffering but rather indications that the body is conserving energy and transitioning toward the final stage of life.
Behavioral and Emotional Signs
Behavioral and emotional signs can be just as telling as physical ones. Some individuals become withdrawn and less responsive, while others may experience restlessness or agitation. Emotional expressions may vary, with moments of clarity or meaningful interaction alternating with long periods of silence. Families often find comfort in continuing to speak to their loved one, offering reassurance and presence even if there is no visible response.
The Final Hours
In the final hours, changes often become more pronounced. Consciousness may fade completely, breathing slows significantly, and the pulse becomes faint. The person may appear peaceful and unresponsive, with eyes partially open or closed. This stage can be deeply emotional for families, but it is also a time when simple acts such as holding a hand, playing soft music, or speaking words of love can provide comfort.
Supporting Your Loved One
Supporting a loved one during this time focuses on comfort care rather than a cure. Keeping the person clean, repositioned, and free from pain is a primary goal. Moistening the mouth, adjusting pillows, and maintaining a calm environment can make a meaningful difference. Communication with the healthcare team is essential, as they can help manage symptoms and explain what to expect. Many families find it helpful to discuss care goals openly, ensuring that treatment aligns with the individual’s wishes and values.
Medical Decision-Making
Medical decision-making becomes especially important when recovery is no longer expected. Understanding treatment options, including life-sustaining interventions, allows families to make informed choices. In many cases, palliative care or hospice care is introduced to focus on quality of life rather than aggressive treatment. These services provide medical, emotional, and spiritual support not only to the patient but also to the family, and they often connect families with resources related to grief and coping.
After Death Occurs
After death occurs, there are immediate steps that healthcare providers can guide families through, such as notifying the appropriate authorities and making arrangements according to cultural or personal preferences. Grief is a deeply personal process, and healing takes time. Seeking support from counselors, support groups, or trusted friends can help families navigate the complex emotions that follow loss.
Recognizing the signs of impending death after a stroke can help families feel more prepared during an incredibly difficult journey. Understanding physical, neurological, and emotional changes allows caregivers to focus on compassion, presence, and comfort rather than fear or uncertainty. While the experience is never easy, awareness and preparation can provide a sense of peace and purpose. For families facing this reality, remember that being there, offering love, and honoring your loved one’s dignity is a powerful and meaningful gift during their final moments.
FAQs About Signs of Impending Death After a Stroke
- How long after a severe stroke do end-of-life signs typically appear?
The timeline varies significantly based on stroke severity, location, and the individual’s overall health. In cases of massive strokes affecting the brain stem or large portions of the brain, signs may appear within hours to days. For less severe strokes, the decline may occur over weeks or months. Medical teams monitor vital signs, consciousness levels, and organ function to assess prognosis. Families should maintain open communication with healthcare providers about what to expect during this difficult time.
- What are the most common physical signs that death may be approaching after a stroke?
Key physical indicators include irregular or labored breathing patterns (such as Cheyne-Stokes breathing), decreased responsiveness or coma, changes in skin color (mottling or cooling of extremities), decreased blood pressure and heart rate irregularities, difficulty swallowing and reduced intake of food and fluids, and decreased urine output. Additionally, patients may exhibit increased drowsiness, withdraw from their surroundings, or experience changes in body temperature. These signs indicate the body’s systems are shutting down, and comfort care becomes the priority.
- Can someone recover after showing end-of-life signs following a stroke?
While rare, some patients do show unexpected improvement even after displaying concerning symptoms. However, when multiple end-of-life signs are present simultaneously—particularly loss of brain stem reflexes, absent response to stimulation, and sustained vital sign deterioration—recovery becomes extremely unlikely. The medical team considers the complete clinical picture, including brain imaging, neurological assessments, and response to treatment. Families facing these decisions should discuss advance directives, quality of life considerations, and care goals with the medical team to ensure the patient’s wishes are honored.
Conclusion and Call to Action
Recognizing the signs of impending death after a stroke is never easy, but this knowledge empowers families to provide compassionate care and make peace with difficult decisions. While we hope you never face such circumstances, understanding these indicators helps ensure your loved one receives dignified, comfort-focused care in their final moments.
Stroke emergencies demand immediate action, and the first few minutes are absolutely critical. Quick, confident intervention can prevent death, minimize brain damage, and significantly improve recovery outcomes. The question isn’t whether an emergency will happen—it’s whether you’ll be ready when it does.
CPR St. Louis empowers you with the life-saving skills that matter most when seconds count. As an American Heart Association training site, we provide comprehensive, hands-on training that builds real confidence for real emergencies.
Take the next step in emergency preparedness:
Protect your community and loved ones by enrolling in CPR certification in St. Louis—master the fundamental techniques that restart hearts and save lives. Healthcare professionals can advance their expertise with our ACLS classes in St. Louis, designed specifically for managing complex cardiac emergencies.
We offer initial certifications and renewals in BLS for Healthcare Providers, ACLS, PALS, and CPR and First Aid. Every course features hands-on practice in a stress-free, supportive environment where you’ll gain genuine skills, not just a card.
Your training today could save a life tomorrow. Register now at CPR St. Louis and be ready when it matters most.





