Respiratory Physiology – outline notes
Call Us Now
Get the Best CPR Class in St. Louis Today!
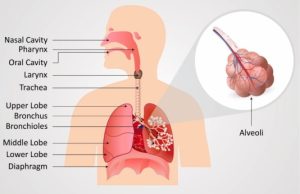
Respiratory System
I. Functions:
A. Provides area for gas exchange between air and blood
B. Moves air to and from area of gas exchange
C. Protects gas exchange surfaces
D. Sound production
E. Provides olfactory sensations to the CNS
F. Capillaries in lungs produce angiotensin converting enzyme (ACE)
II. 4 Respiratory processes
A. Pulmonary ventilation (breathing)
1. Move air in and out of lungs
B. External respiration
1. Gas diffusion across respiratory membrane
2. O2 loading / CO2 unloading
C. Internal respiration
1. Gas diffusion to tissues of the body
2. O2 unloading / CO2 loading
D. Transport of O2 and CO2
III. Pulmonary ventilation
A. Movement of air in/out to maintain alveolar ventilation
B. Boyle’s Law
1. Inverse relationship b/t Pressure and Volume
2. P1V1=P2V2
3. P = 1/V
4. If you double the external pressure on a flexible container, its
volume will drop by half : If you reduce the external pressure
by half, the volume of the container will double
C. Air flows from high to low Pressure
D. Mechanisms of Pulmonary Ventilation
1. Inhalation
a. Diaphragm contracts, rib cage in elevated
b. Pressure in lungs decreases due to increase volume
c. Air flows in from high to low pressure
2. Exhalation
a. Pressure in lungs increases due to volume decrease
b. Air moves out from high to low pressure
E. Compliance
1. Expandability of lungs
2. Anything decreasing lung compliance will make it more difficult
to fill and empty them
a. Increased alveolar surface tension
b. Decreased mobility of thoracic cage
F. Resistance to gas flow – friction in airways
1. Gas Flow = ∆P / resistance
2. Asthma
G. Pressure changes during breathing
1. Atmospheric pressure = 760 mm Hg
2. Intrapulmonary pressure (intra-alveolar)
a. Pressure inside alveoli
b. 759 mm Hg during inhalation (-1 mm Hg)
c. 761 mm Hg during exhalation (+1 mm Hg)
d. Valsalva maneuver
3. Intrapleural pressure
a. Pressure in pleural cavity
1) Between visceral and parietal pleurae
b. Averages –4 mm Hg
c. Negative pressure due to:
1) Elastic fibers pulling lungs away from chest wall
4. Pneumothorax – entry of air into pleural cavity
a. breaks fluid bond of pleurae
b. atelectasis – lung collapse
H. Modes of Breathing
1. Quiet breathing
a. Inhalation – muscle contraction
b. Exhalation – passive (elastic rebound)
—————————-
c. Deep breathing – use diaphragm
d. Shallow breathing – external intercostals
1) Pregnancy – due to pressure on diaphragm
2. Forced breathing
a. Accessory muscles
IV. Respiratory Rates and Volumes
A. Respiratory minute volume (VE) – ml / min
1. VE = Respiratory rate (f) x Tidal volume (VT)
2. 6.0 L = 12 breaths/min x 500 ml
Call Us Now
Get the Best CPR Class in St. Louis Today!
B. Alveolar ventilation (VA)
1. VD – anatomic dead space
a. 150 ml of tidal volume never reaches alveoli
2. VA = f x (VT – VD)
3. 4.2 L = 12 x (500 – 150)
C. Overhead of Volumes and Capacities
V. Gas Laws
A. Partial Pressure (Dalton’s Law)
1. Total pressure exerted by a mixture of gases is the sum of
individual pressures exerted by each gas.
2. Sum of partial pressures = total pressure
3. O2 = 21% —— .21 x 760 mmHg = 159 mmHg
4. N2 = 78.6% ——– pp = 597
B. Henry’s Law
1. Amount of gas in solution is proportional to pp of that gas
2. At gas and liquid contact – gas under pressure will force
gas into liquid until equilibrium
3. Ex) soda under pressure in can until opened
4. At given pp and temp – gas solubility determines am’t of
gas in solution
5. CO2 is 20 times as soluble as O2
* In a pulmonary vein
-2.62 ml/dl of CO2 (pCO2 = 40 mmHg)
-0.29 ml/dl of O2 (pO2 = 100 mmHg)
-1.25 ml/dl of N2 ( pN2 = 573 mmHg)
6. Pressure = [dissolved gas] / Solubility coefficient
7. Solubility coefficients
a. O2 = 0.024
b. CO2 = 0.57
c. N2 = 0.012
C. Diffusion (D) of gases
D = ∆P x A x S / d x √MW
∆P – pressure difference
A – cross-sectional area
S – solubility of gas
D – distance
MW – molecular weight of gas
VI. External Respiration – at lungs
A. Inhaled air
1. Nasal cavity – warms, humidifies, filters
2. Mucus escalator – trachea
3. Alveolar macrophages (Dust Cells)
4. Air mixes with old alveolar air
B. Diffusion across respiratory membrane
1. Endothelium of alveolus (Type I cells)
2. Endothelium of capillary
3. Surfactant layer inside alveoli
a. Surfactant – produced by Type II (septal cells)
1) Decreases surfaced tension
b. Distance is small (0.5 µm)
1) Affected by pneumonia
4. pp gradient determines movement
a) Light headed at high altitudes (low pp of O2)
5. Large surface area
a) Emphysema
VII. Internal respiration – at systemic tissues
1. OVERHEAD
2. Exchange between systemic capillaries and tissue
3. Review capillary exchange
VIII. Gas Transport – Oxygen
A. Oxygen has low solubility
1. 100 ml of blood (alveolar capillaries)— 20 ml of O2
a. 0.3 ml of dissolved O2 (1.5%)
b. 98.5 % – bound to Hemoglobin (iron in Heme group)
2. Hemoglobin saturation
a. 4 O2 = 100%
b. 2 O2 = 50%
c. Hb binds O2 reversibly
B. Oxygen-Hemoglobin dissociation curve
1. Relates saturation of Hb with pO2
2. increase pO2 —— increase Hb saturation ( ↑ affinity)
a. Hb stores O2
3. decrease pO2 —– decrease Hb saturation (↓affinity)
a. Hb releases O2
4. Normal tissue
a. 97% (pO2 = 95 mmHg) —– 75% (pO2 = 40 mmHg)
b. Venous blood has large O2 reserve
5. Active tissue
a. drops to 20% saturation (pO2 = 15-20 mmHg)
b. uses 3.5 more O2
6 Carbon Monoxide (CO) poisoning
C. Hemoglobin and pH
1. Bohr Effect
a. systemic tissue – decrease pH —— ↓Hb affinity for O2
b. CO2 + H2O — H2CO3 – H+ + HCO3-
c. ↑H+ —- ↓pH – ↑acid
d. lungs – ↓pCO2 — ↑Hb affinity for O2
D. Hb and Temperature
1. ↑Temp —- ↓ Hb affinity for O2
2. Active skeletal muscle
E. Hb and 2,3-bisphosphoglycerate (BPG)
1. ↑ BPG —- ↓ Hb affinity for O2
2. BPG produced by RBC metabolism
3. Increase production at ↑pH (acidosis inhibits glycolysis in RBC)
4. Bohr effect improves O2 delivery at ↓pH
IX. Gas Transport – Carbon Dioxide
A. 3 Modes of transport
1. Carbaminohemoglobin – 23%
a. CO2 binds to -NH2 group (globin portion)
2. Dissolved in plasma – 7%
3. Bicarbonate ion (HCO3-) – 70%
a. CO2 + H2O — H2CO3 – H+ + HCO3-
b. Carbonic anhydrase in RBC
c. H+ binds to Hb (buffer)
d. HCO3- diffuse out of RBC to plasma and back to lungs
1) Chloride shift – Cl- exchanged for HCO3-
B. Haldane effect
1. Binding of O2 to Hb (causes Hb to become a stronger
acid) in lungs results in removal of CO2
2. In tissue capillaries, release of O2 increases binding of
CO2