Necrotizing Fasciitis by Tzipporah Weiss
Call Us Now
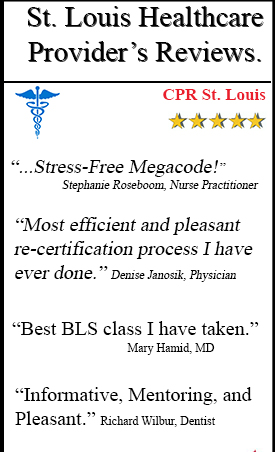
Get the Best CPR Class in St. Louis Today!
Necrotizing fasciitis is a rare but life-threatening aggressive soft-tissue infection that causes rapidly spreading inflammation and the death of the soft-tissue (necrotizing) and the fascia, the layer of soft tissue covering the muscle. This is also commonly known as flesh-eating disease or flesh-eating bacteria syndrome. Infection typically follows trauma, although may be as minor as a scrape or an insect bite. Often necrotizing fasciitis is caused by toxin-producing, virulent (aggressive) pyogen (pus producing) bacteria called group A (A- antigen) streptococcus (twisted, sphere shaped bacteria) and it is frequently accompanied by severe poisoning of the whole system or organism. This condition can be fatal without immediate recognition and aggressive surgical treatment. Necrotizing fasciitis is often first misdiagnosed as a benign (non cancerous) soft-tissue infection. Surgical debridement is the single most influential course of action to deter mortality. Important treatments for this life- threatening infection would be prompt diagnosis, antibiotics and aggressive surgical debridement of affected tissue.
Lets start by breaking down the term necrotizing fasciitis into its simplest form to understand what we are talking about. The literal definition of the word necrotizing is causing the death of a specific area of tissue and fasciitis meaning the inflammation of a fascia. As defined by Definition.com, a fascia is a flat band of tissue below the skin that covers the underlying tissues and separates different layers of tissue. Necrotizing fasciitis is a rare, systemic toxin- spreading infection of the deep layers of skin, tissue or muscle.
The bacterial infection causing necrotizing fasciitis that I am choosing to focus on is Group A Streptococcus (GAS), which is a bacteria that ranges from moderate superficial skin infections to life-threatening systemic diseases. Group A streptococci spread their bacteria via direct contact from mucous droplet of those already affected such as strep throat or through site of trauma, like surgery or even a non- apparent, minor scratch or bite. This bacteria thrives anaerobically (without oxygen), grows and colonizes in pairs in your body. Bacterias like GAS typically grow in warm moist environments and when entered into a person give off toxic gases and spread rapidly. If the dead tissue is not removed the bacteria multiplies and gives off toxins and enzymes that destroy the soft tissue and fascia which eventually kills the tissue. The bacteria thrives anaerobically in the dead tissue therefore the pus and the dead tissue need to be removed promptly. A surgeon must go in and surgically open up and expose the bacteria to oxygen and remove and flush out the destructive tissue before a systemic disaster occurs. Usage of antibiotics is important as well.
Which groups of people are more likely to get this disease? Over 70% of cases are recorded in patients with one of the following clinical situations: immunosuppression (immune deficiency), diabetes, alcoholism/drugs and chronic systemic diseases such as cancer, diabetes, chronic heart disease, lung disease and those on medications such as steroids and chemotherapy. Also the young or elderly patients are at higher risk and people with skin lesions (such as cuts, burns and surgical wounds). It occasionally occurs in people with an apparently normal general condition.
Necrotizing fasciitis symptoms may include intense pain. With progression of the infection, often only hours the tissue becomes swollen. If it is early on, bacteria may be deep within the tissue therefore there will be no signs of inflammation apparent. If the bacteria is superficial the patient may immediately experience hot skin, redness and swelling, all signs of inflammation. The death of the tissue may cause blisters on the skin.
The identification of the nature of the illness by examining the symptoms would include microscopic evaluation of tissue samples; powerful broad- spectrum antibiotic treatments immediately inserted via IV until culture results have been proven positive. Once indicated positive, surgery is required to open and expose the tissue to oxygen, drain the fluid from the infected area and removal of infected tissue. By the surgeon removing the infected tissue it is in fact saving the healthy soft tissue and keeping the infection and toxins from spreading.
Administering penicillin and clindamycin is recommended. Nurses should be wary to watch the patients heart rate that it is not going too fast(tachycardia), the white blood cell count is not too high (leukocytosis), their pulse does not let too weak, and that the infection has not become systemic.
All in all, necrotizing fasciitis refers to an aggressive, fast spreading infection across the fascial planes, resulting in the death of the tissue (necrosis). A common bacteria causing necrotizing fasciitis is Group A streptococci bacteria which invades the body, lets off systemic toxins and damages and kills tissues. The bacteria thrives off of dead tissue therefore it is very important to involve surgical debridement. The surgeon needs to open up the skin, expose the bacteria to oxygen and remove the dead tissue and pus and to wash it out. Admission of fluids and antibiotics via IV are important. Necrotizing fasciitis left untreated is fatal.
Sources:
Cdc.gov Group A Streptococci bacteria
Emedicine.medscape.com
Phil.cdc.gov
Podiatry Today Magazine
Niaid.nih.gov
Pathmicro.med.sc.edu Streptococci
Call Us Now
Get the Best CPR Class in St. Louis Today!